Hemocytoblasts, or multipotent hematopoietic stem cells, give rise to myeloid stem cells, which differentiate into myeloblasts, megakaryocytes, and red blood cells (erythrocytes). Red blood cell production is regulated by the hormone erythropoietin, which is produced by cells in the kidneys and liver.
Mature red blood cells are flexible, oval or round biconcave discs that move easily through the blood vessels. Certain pathologies, such as sickle-cell anemia, alter the shape and flexibility of red blood cells, making it difficult for them to move smoothly through blood vessels.
Unlike most other eukaryotic cells, mature red blood cells don’t have nuclei. When they enter the bloodstream for the first time, they eject their nuclei and organelles, so they can carry more hemoglobin, and thus, more oxygen.
Each red blood cell has a life span of around 100–120 days. Old, dead, or damaged red blood cells are engulfed by phagocytic cells in the liver, spleen, and lymph nodes. The iron from these cells is subsequently recycled to produce new hemoglobin.
Hemoglobin is the protein that makes it possible for red blood cells to carry oxygen. Each molecule of hemoglobin is made up of four protein chains. Each chain has a heme group that contains an iron atom. Oxygen can bind to these iron atoms, which means that one molecule of hemoglobin can carry four oxygen molecules. The bond between oxygen and the iron contained in hemoglobin’s heme groups is what makes oxygenated blood red.
In the lungs, the hemoglobin in the red blood cells picks up oxygen. Then, the heart pumps the oxygenated blood out through the aorta, moving it through arteries and capillaries to reach the body’s tissues.
After the hemoglobin releases its oxygen molecules into the body’s tissues, it can form bonds with some of the carbon dioxide (CO2) absorbed into the bloodstream. However, hemoglobin does not carry all the carbon dioxide in the blood back to the lungs—the blood can also transport CO2 as a dissolved gas or as bicarbonate (HCO3).
When inhaled, carbon monoxide (CO) binds to hemoglobin’s heme groups. When this happens, it prevents oxygen from binding to the heme groups, and therefore, the hemoglobin can’t carry oxygen to the body’s tissues. As a result, carbon monoxide poisoning can cause permanent damage to the brain and/or heart, and it can be fatal.
Like red blood cells, platelets are derived from myeloid stem cells. Some of these stem cells develop into megakaryoblasts, which give rise to cells called megakaryocytes in the bone marrow. After a megakaryocyte has matured, pieces of its cytoplasm break away into cell fragments called platelets. A single megakaryocyte can produce 1000–3000 platelets. Because they are not cells, platelets don’t have their own nuclei. However, they do contain numerous granules (or vesicles).
The hormone thrombopoietin, produced by the liver and kidneys, regulates the production of megakaryocytes and platelets.
Platelets have different appearances in their inactivated and activated states. When inactivated, platelets are irregularly shaped discs. Activated platelets are spherical, with protrusions that allow them to stick to wound tissue and to other platelets to form a plug at the site of a blood vessel tear. Activated platelets also release chemicals from their granules to initiate clotting.
The life span of a platelet is about 10 days. Like red blood cells, old platelets are phagocytosed. Reserve platelets are stored in the spleen.
When a blood vessel tears, platelets adhere to the (damaged) blood vessel wall near the tear, forming a platelet plug. At this point, they change from their inactive to their active shape, and they empty the contents of their granules.
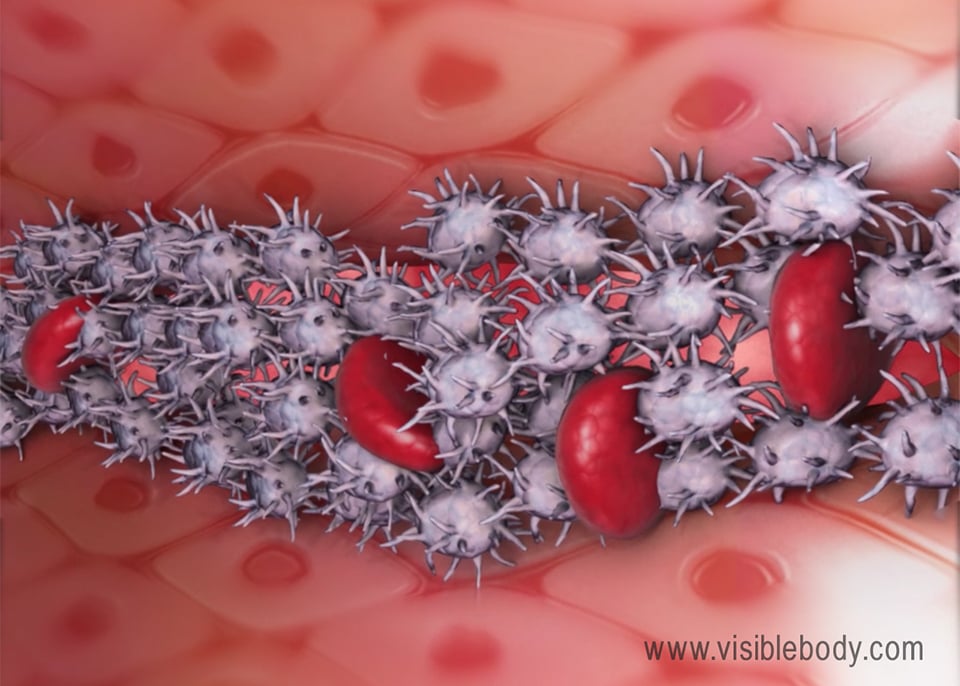
At the site of an injury, the platelets connect to one another and release chemicals that stimulate blood clotting. Proteins called clotting factors form fibrin threads that, together with the platelets, form a clot.
Articles about and visualizations of hemoglobin from Kenyon College and PDB-101.
Information about carbon monoxide poisoning from the Mayo Clinic.
Information about sickle cell anemia from the Mayo Clinic.
Notes on hematopoiesis from Austin Peay State University’s biology site.
UCSB ScienceLine: Why is blood red?
When you select "Subscribe" you will start receiving our email newsletter. Use the links at the bottom of any email to manage the type of emails you receive or to unsubscribe. See our privacy policy for additional details.